The hospitals where waiting times are getting worse. Is yours one of them?
Nearly a quarter of hospital trusts in England have seen waiting times deteriorate in the past year.

Nick Triggle,Health correspondentand
Daniel Wainwright,BBC Verify
 Getty Images
Getty ImagesNearly a quarter of hospitals in England have seen waiting times worsen since the government published its plan to tackle the backlog a year ago, BBC analysis shows.
Hitting the 18-week waiting target for treatments such as knee and hip operations was Labour’s key manifesto pledge for the health service, and last January it set out how it would get hospitals on track.
While nationally progress is being made, 31 hospital trusts have gone backwards and another 17 have made little progress out of the 129 services examined.
The hospitals struggling the most said they were facing a variety of challenges, including staffing shortages, doctor strikes and problems with IT systems.
‘Living in pain’
Mary Waterhouse, 72, from Blackpool, is one of many patients who has faced delays at a hospital where waits are getting worse.
She has arthritis and has been receiving treatment from Blackpool Hospitals NHS Trust since 2022. She was initially given steroid injections, but was referred back on to the waiting list in late 2024 as her condition worsened.
She had to wait eight months to get assessed, but by that point her health had deteriorated so much she was told she would need hip and knee replacements on both sides.
 Arthritis UK
Arthritis UKShe opted against treatment. “My arthritis was too advanced – and it was too many operations. I have decided to live with the pain. I had long waits at every stage since first being referred. It’s like being in a never-ending queue.
“I now rely on a mobility scooter to get about – I can only walk short distances with crutches. If I had received quicker treatment, things may have been better.”
Deborah Alsina, of Arthritis UK, said Mary’s case was typical of the problems being faced by many thousands of people with arthritis.
She said timely treatment can be “life-changing”, but there was not equitable access to care.
Blackpool said it could not comment on Mary’s case, but chief executive Maggie Oldham acknowledged waits were too long.
“We know we’re not where we need to be, but we’re continuing to work hard alongside our partners to address the issues we’re facing urgently.”
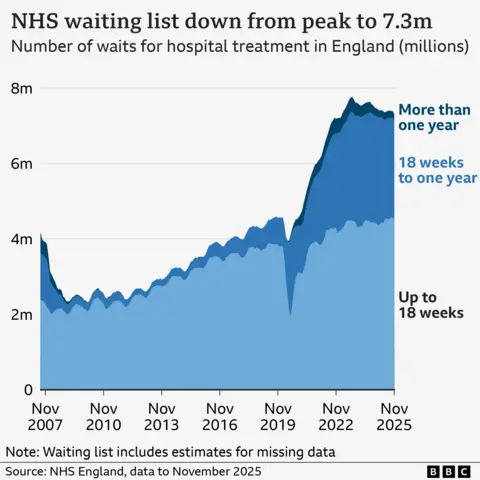
The government has made improving waiting times its key priority for the NHS and has pledged to get back to hitting the 18-week waiting time target in England by March 2029. It has not been met since 2015.
The target requires 92% of patients to be seen in 18 weeks. An interim national target of 65% has been set for March 2026.
When the government published its plan last January, 59.2% of patients were waiting less than 18 weeks; that has now improved to 61.8%. The size of the waiting list has also fallen to 7.31 million – the lowest level since February 2023.
But locally there are big differences in performance, despite dedicated funding having been set aside to help NHS trusts – which have been given their own individual targets for improvement.
The BBC was able to compare current performance with the position 12 months ago at all but two hospital trusts – data was not available for Sheffield and Barking, Havering and Redbridge hospital trusts.
While published in January, the data lags by a couple of months so marks the position at the end of November in both 2024 and 2025.
East Cheshire has had the biggest drop, going from 61.2% of patients waiting less than 18 weeks to 51.2%.
Barnsley saw a drop of nine percentage points, while both Whittington Health and Epsom and St Helier NHS trusts experienced falls of around five percentage points.
NHS trusts said a variety of factors were at play. Epsom and St Helier cited the introduction of a new electronic patient record system which disrupted services, while Barnsley said staff shortages and an increase in cancer referrals which had to be prioritised ahead of planned treatments had caused problems.
Strike action by resident doctors was also blamed – the number of doctors walking out during industrial action has varied from place to place.
Barnsley and Epsom and St Helier both said they expected performance to start improving.
Of the 98 that had seen progress in the past year, 17 had only improved by less than one percentage point.
But some had seen big jumps. Five NHS trusts recorded improvements of between nine and 10 percentage points and Shrewsbury and Telford, which was one of the worst performers a year ago, by 17.
‘Stark differences’
The 18-week pledge only applies to England, but targets for hospital treatments are being routinely missed in other parts of the UK.
Rory Deighton, of the NHS Confederation, which represents NHS trusts, said: “The NHS is not one homogenous body but is made up of hundreds of separate organisations, each with their own distinct financial and operational challenges.
“This means that tackling care backlogs will be more difficult in some parts of the country than others – particularly if there are entrenched challenges, such as high levels of local deprivation.”
Chris McCann, deputy chief executive at patient watchdog Healthwatch England, said the analysis showed there were “stark differences” for patients depending on where they live.
“Those responsible for monitoring NHS trusts must pay close attention to organisations that are not only performing poorly but actually deteriorating,” he added.
A Department of Health and Social Care spokeswoman said the government had got the NHS on the “road to recovery” but there was still more to do.
She said investment was being made in services such as new surgical hubs and evening and weekend scanning, which would help.
And she said individual hospitals would be held to account for their performance.